What is vascular Ehlers-Danlos Syndrome?
Vascular Ehlers-Danlos Syndrome (vEDS) is a rare disorder that weakens the body’s connective tissue. Connective tissue is like a glue that supports different parts of the body, like the skin, eyes, and heart. It gets its strength from a proteinA large molecule inside a living thing made up of amino acids. called collagen. Normally, collagen keeps the tissue elastic and able to stretch without tearing. Weakened connective tissue can lead to less serious complications like bruising, or more serious events like rupturesThe tearing apart of a tissue. in arteriesA tube-shaped vessel that carries blood from the heart throughout the body., intestines, and hollow organs, like the uterus and bowel.
What causes vEDS?

A geneA part of a cell that controls the traits of a living thing. called COL3A1 plays a central role in producing type III collagen, a major protein present in the walls of blood vessels and hollow organs. For people with vEDS, a mutation in the COL3A1 gene leads to defects in type III collagen and/or reduced amounts of type III collagen. There are different types of genetic variations that can determine the characteristics and severity of vEDS caused by this mutation. This defect in the COL3A1 gene is what causes vEDS.
Experts estimate there are as many as 5,000 Americans with vEDS. Roughly 2,000 cases are known at this time.
What are the signs and symptoms of vEDS?
Every person with vEDS is different, but there may be signs seen in your medical history:
- Aneurysms, dissection, or rupture in arteries
- Rupture in intestines
- Rupture in uterus during pregnancy
- A collapsed lung
- Dislocated hip (at birth)
- Family history of vEDS
Visual similarities are often seen across vEDS patients:
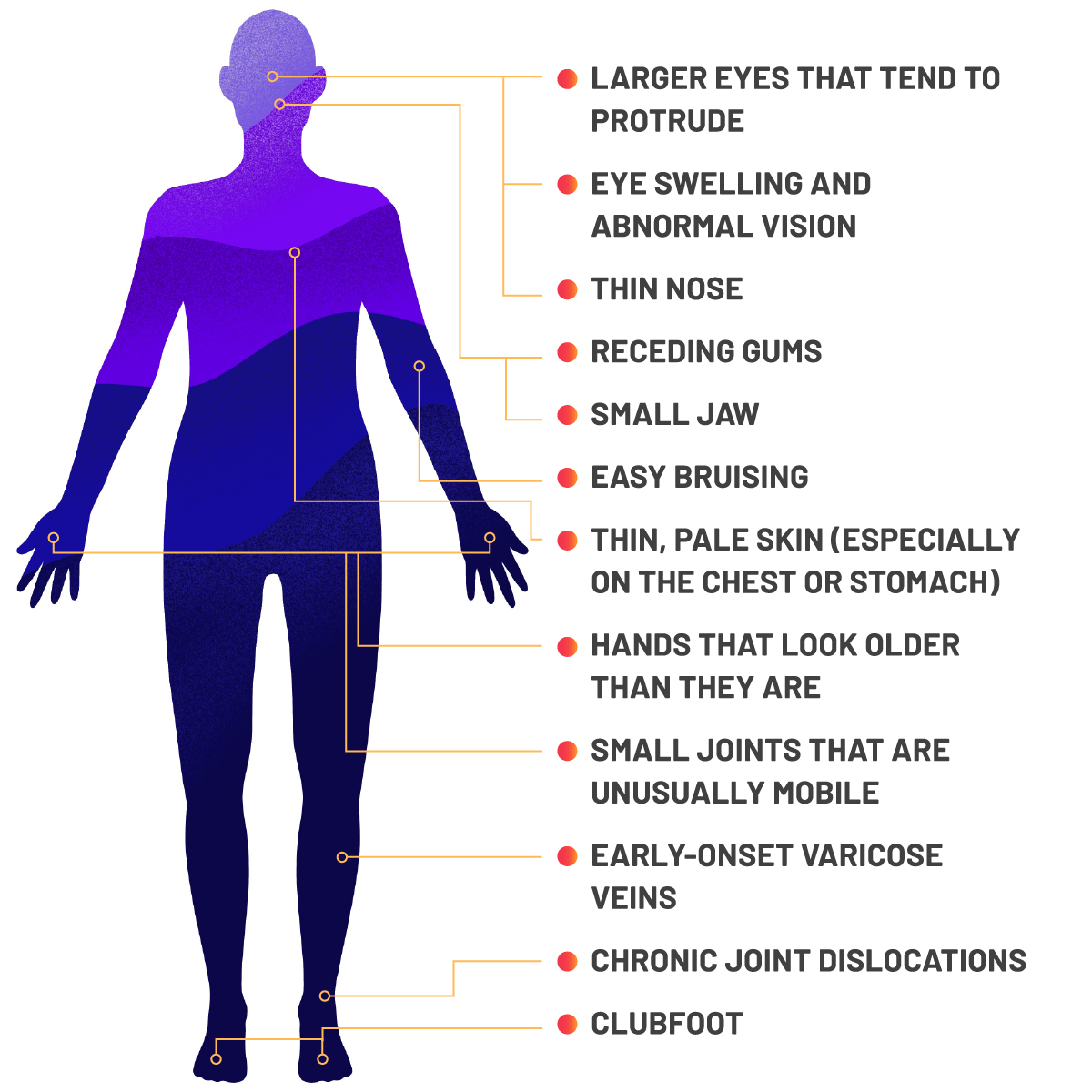

- Large eyes that tend to protrude
- Eye swelling and abnormal vision
- Thin nose
- Receding gums
- Small jaw
- Easy bruising
- Thin, pale skin (especially on the chest or stomach)
- Hands that look older than they are
- Small joints that are unusually mobile
- Early-onset varicose veins
- Chronic joint dislocations
- Clubfoot
Your symptoms alone will not confirm a vEDS diagnosis. Talk to your doctor about confirmation with genetic testing.
How is vEDS diagnosed?
vEDS is sometimes suspected based on clinical signs or eventsEvents can include aneurysms, arterial dissection or uterine rupture., and usually only after a major vascular event. Since vascular EDS can look like other rare aortic conditions like Loeys-Dietz syndrome, Marfan syndrome, or familial arterial aneurysm and dissection syndromes, vEDS should be confirmed with a genetic test.
Not every doctor tests for vEDS. You may need to tell your doctor that you would like to be referred to a lab to confirm your diagnosis through testing.
vEDS affects both males and females.
What are the complications of vEDS?
Complications can include arterial ruptures and dissectionsA splitting or separation of tissue due to disease., spontaneous bowel perforationsA rupture in the gastrointestinal wall., and organ ruptures.
Up to a quarter of people with vEDS experience their first related medical complication by age 20. By the time they get to 40 years of age, more than 80% may have suffered a major vEDS-related arterial event.
How is vEDS managed?
The goal for the management of vEDS should be to ensure the likelihood of serious events is minimized to maintain the best quality of life possible. While there is currently no cure for vEDS, there are ways to manage it.
Take Extra Precautions
Some activities can be harmful for people with vEDS. Talk to your vEDS specialist about the risks associated with the following activities and medical treatments:
- Collision sports, heavy lifting, and weight training that could cause traumaAny harm caused by an outside force.
- Elective surgeryAny surgery that is beneficial to the patient but not essential for survival.
- Routine colonoscopiesAn examination of the large intestine and a part of the small intestine with a camera on a flexible tube that is passed through the anus.
- ArteriogramsA procedure that produces images of a patient’s arteries.
Monitor Your Body
Your vEDS specialist may be able to monitor the potential risk of a major vascular event using:
- Arterial ultrasoundsA noninvasive technique involving the formation of a two-dimensional image used for the examination of a patient’s arteries and measurement of internal body structures.
- Magnetic resonance angiograms (MRAs)A noninvasive technique that creates images of the heart, blood vessels, or blood flow.
- Computed tomography (CT) angiogramsAn X-ray scan of the blood vessels.
The potential risks and benefits of each of these procedures should be discussed with your vEDS specialist.
Ask your vEDS specialist to monitor your blood pressure on a regular basis to allow for early treatment if hypertension develops.
What is the life expectancy for someone with vEDS?
It can range anywhere from 10 to 80 years, with an average of 51 years. This means half of all US patients live to be over 51 years old.
What impact can vEDS have on family planning?
Something else to consider, is the fact that vEDS can be inherited.

Pregnancy can cause life-threatening complications for women with vEDS due to the fragile tissues and reproductive organs caused by the disorder.
If you are pregnant or think you might become pregnant, talk to your doctor or OB/GYN to understand your personal risks and how best to manage them.

